Background: Patients (pts) treated with intensive induction therapy for newly diagnosed acute myeloid leukemia (AML) traditionally remain admitted until an absolute neutrophil count (ANC) >0.5 x 10 3/L. Although a small number of centers reported on pt discharge with ANC <0.5 x 10 3/L via an “early” discharge (DC) program (EDP) post-intensive induction, little is known about the safety and outcomes among this group of pts, including the rates and predictors of post-DC complications (e.g., febrile neutropenia (FN), microbiologically proven infection) and both early- and long-term outcomes. We sought to describe our experience with an EDP and identify predictors of differential outcomes.
Methods: We conducted a single-center, retrospective study of pts with newly-diagnosed AML admitted to Yale Cancer Center (YCC) for intensive induction during December 2014-January 2023. Re-induced patients were excluded. Patients were eligible for the EDP if they: 1) were afebrile x 7 days, 2) required no parenteral therapies, 3) required transfusion support less than daily, 4), lived within 60 minutes of YCC with “average” traffic, and 5) had a dedicated care giver available 24 hours per day with reliable transportation to/from clinic. Chi-square and Wilcoxon rank-sum tests were applied to categorical and continuous variables, respectively. Overall survival (OS) was estimated using the Kaplan-Meier method and was compared using log-rank test. Statistical significance was determined by p-value <0.05.
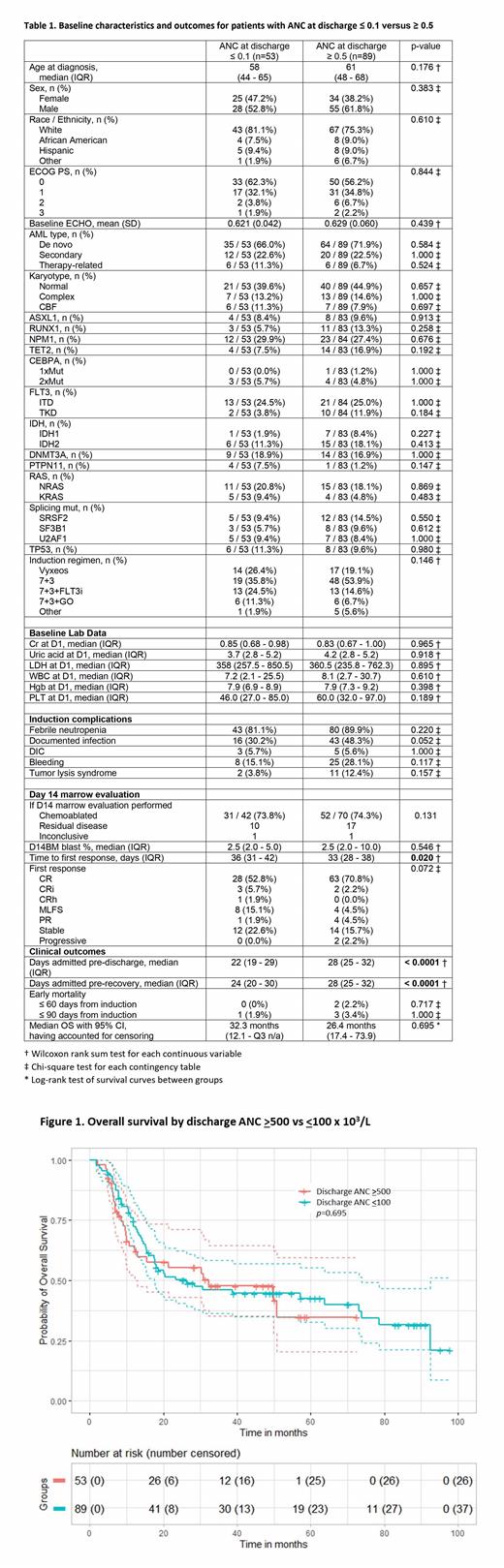
Results: A total of 188 pts were evaluated. Amongst this population, 99 (52.7%) pts were DC under the EDP, while 89 (47.3%) were not. To remove confounding from peri-DC ANC kinetics, we focused on pts DC with an ANC <0.1 x 10 3/L (n=53, “EDP pts”) and compared them with non-EDP pts (DC ANC >0.5 x 10 3/L). There were no significant differences in age, sex, ECOG performance status (PS), baseline LVEF on echocardiography or other comorbidities. With regards to disease-specific factors, there was no difference in pre-induction blood counts (e.g., WBC 7.2 vs. 8.1, p=0.610), serum creatinine, uric acid, lactate dehydrogenase, AML subtype, or disease biology e.g., karyotypic or molecular features (Table 1).
Pts received 7+3 without (47%) or with (27%) other therapy, while 22% received liposomal daunorubicin/cytarabine. There were no differences in the rates of regimens used between EDP and non-EDP pts. The incidence of induction-related complications like FN (81.1% vs 89.9%, p=0.220), DIC, TLS, and bleeding were similar between groups, although there was a trend toward more documented infection among non-EDP pts (48.3% vs 30.2%, p=0.052). Findings on the D14 marrow (performed in 79% of pts) were similar between groups (chemoablation, p=0.131; D14 blast %, p=0.546).
Median days admitted from induction to DC was nearly a week less for EDP pts (22 [interquartile range (IQR): 19-29] vs 28 days [IQR: 25-32], p<0.0001). Amongst EDP patients, 12 (22.6%) were re-admitted, 10 (83%) due to FN with 4 of these pts having an infectious source identified. The median duration of re-admission was 6.5 days (IQR: 4.5-13). When considering re-admissions prior to ANC/count recovery or initiation of consolidation, EDP pts still had lower time spent in hospital prior to eventual count recovery (24 vs 28, p<0.0001).
ANC at DC did not predict OS amongst the larger cohort (n=188, p=0.949), but was associated with re-admission amongst pts DC with ANC <0.5 in univariate analysis ( p=0.02). Time to DC and ANC at DC were strongly associated amongst the larger cohort (n=188, p=0.01 from linear regression) and pts DC with ANC <0.5 ( p<0.00001 from linear regression)(Figure 1).
Although non-EDP pts had a shorter time to first response (33 vs 36 days, p=0.020), there were no differences in rates of CR/CRi/CRh (73.0% vs 60.4%, p=0.167) when compared with EDP pts. Similarly, there were no differences in early (60- and 90-day) mortality, or median OS between EDP and non-EDP pts (32.3 vs 26.4 months, p=0.695)(Table and Figure 1).
Conclusions: Our study shows that pts treated intensively for newly-diagnosed AML and meeting several criteria can be safely DC prior to count recovery without detriment to early mortality or OS. EDP pts spent up to a week more out of hospital when compared with non-EDP counterparts. Healthcare utilization, cost effectiveness and patient satisfaction evaluations of the EDP are underway.
Disclosures
Podoltsev:Cogent Biosciences: Other: IDMC Member; AI Therapeutics; Arog Pharmaceuticals; Astellas Pharma, Inc.; Astex Pharmaceuticals; Boehringer Ingelheim Pharmaceuticals, Inc.; Celgene Corporation; CTI BioPharma Corp.; Daiichi Sankyo, Inc.; Genentech, Inc.; Jazz Pharmaceuticals, Inc.; Kartos Therapeuti: Research Funding; AbbVie Inc.; Blueprint Medicines (former); Constellation Pharmaceuticals (former); CTI BioPharma Corp. (former); Incyte Corporation (former); Novartis (former); PharmaEssentia (former): Consultancy. Zeidan:Schrödinger: Consultancy, Honoraria; Syndax: Consultancy, Honoraria; Genentech: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; ALX Oncology: Consultancy, Honoraria; Lox Oncology: Consultancy, Honoraria; Regeneron: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; BeyondSpring: Consultancy, Honoraria; Agios: Consultancy, Honoraria; Jazz: Consultancy, Honoraria; Notable: Consultancy, Honoraria; Orum: Consultancy, Honoraria; Kura: Consultancy, Honoraria; Chiesi: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Epizyme: Consultancy, Honoraria; Syros: Consultancy, Honoraria; Shattuck Labs: Research Funding; Otsuka: Consultancy, Honoraria; Daiichi Sankyo: Consultancy, Honoraria; Boehringer-Ingelheim: Consultancy, Honoraria; Servier: Consultancy, Honoraria; BioCryst: Consultancy, Honoraria; Zentalis: Consultancy, Honoraria; Geron: Consultancy, Honoraria; Ionis: Consultancy, Honoraria; Taiho: Consultancy, Honoraria; Tyme: Consultancy, Honoraria; Foran: Consultancy, Research Funding; Mendus: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Astex: Research Funding; Celgene/BMS: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Janssen: Consultancy, Honoraria. Shallis:Bristol Myers Squibb: Consultancy; Curio Science: Consultancy; Servier: Consultancy; Rigel: Consultancy; Gilead Sciences: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal